Written by Dr Debbie Pu, Research Fellow, Monash University, and Michele Conlin, Research Translation Coordinator, East Grampians Health Service
What questions did we ask?
Residential In-Reach (RIR) programs are designed to provide specialist consultative care for residents in residential aged care facilities (RACFs) with the aim of avoiding unnecessary hospital transfers and providing post hospitalisation support. RIR programs are one of the priority funding areas for the Victorian Department of Health. There is also support from Safer Care Victoria to engage different stakeholders to inform health service partnerships that plan to undertake clinical redesign for RIR programs.
The Grampians Region Health Service Partnership and its RIR Redesign Committee are interested in examining the evidence base for potential RIR programs in the region. The following questions were asked:
– What models of residential in-reach are described in the literature?
– What are the reported strengths & weaknesses of these models?
What were the findings?
Most RIR programs identified were Australian, with the exception of one based in Finland and another in the UK. The majority were located in urban areas (11 studies), though three programs were run out of multiple areas of mixed density, and four were based exclusively in rural or regional areas. Studies generally included multiple RACFs in their samples (median of 16.5, range 1-85).
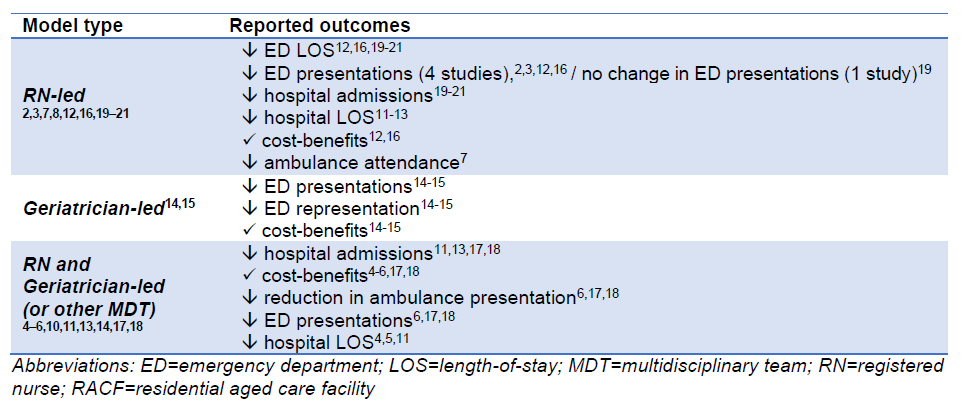
Findings were summarised by intervention components and reported outcomes:
An overview of model strengths and weaknesses, including those related to implementation, were synthesised and can be found in the Summary document.
What does this mean for health services and clinicians?
Based on the evidence included in this rapid synthesis, the following insights were formed for consideration when designing and implementing RIR programs:
– Three types of RIR programs (RN- or geriatrician-led, or with a multidisciplinary organisation) have been evaluated and all have the potential to decrease ED presentations of acutely unwell residents living in care facilities compared to usual care without RIR support.
– There is some evidence that implementing a RIR model of care leads to cost benefits for health services (9/18 studies).
– There is limited evidence on the implementation of RIR in regional and rural settings (only 4/18 included studies). Adoption of RIR models implemented in urban settings may need adapting for the rural and regional context where there are unique challenges including access to healthcare, workforce shortages, barriers to the use of IT and telehealth, and long distances between health services and RACFs. Health services could partner with experienced implementers who can draw on implementation science to plan for tailored implementation.
Read the Rapid Evidence Summary here.